The integumentary system is the group of organs including skin and skin-derived organs, such as epithelial glands, hair and nails.
The Skin
Skin is the largest and heaviest organ of the body. It has three primary layers: 1) epidermis, the skin’s outermost layer, is thin and continuously sheds dead skin cells; 2) dermis is the middle layer and has sweat glands, blood vessels, nerves, and hair follicles; 3) hypodermis is the innermost layer comprising connective tissue and adipose tissue that connects the skin to the muscles beneath and provides insulation and cushion. Depending on the thickness of the skin, particularly the layers of the epidermis, two types of the skins can be distinguished, i.e., thick skin and thin skin.
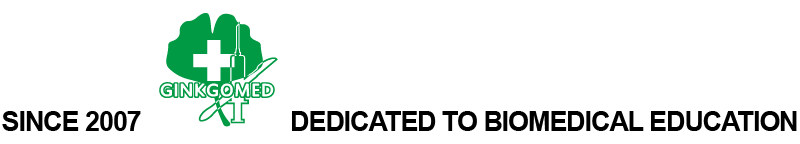
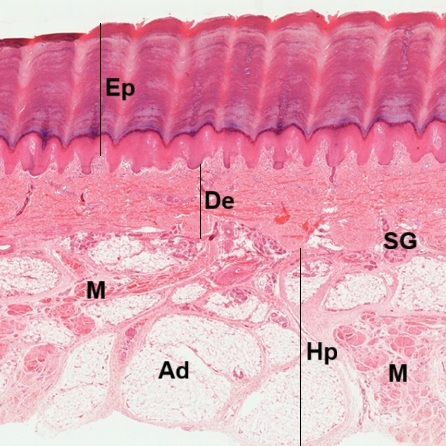
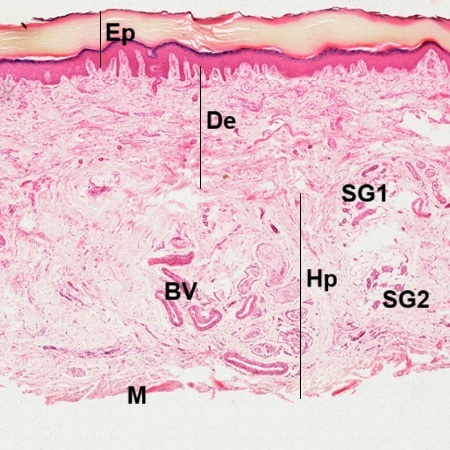
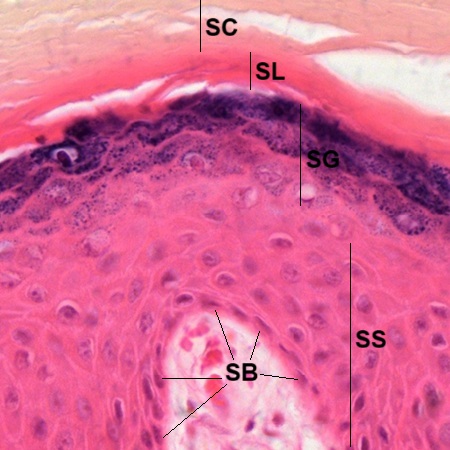
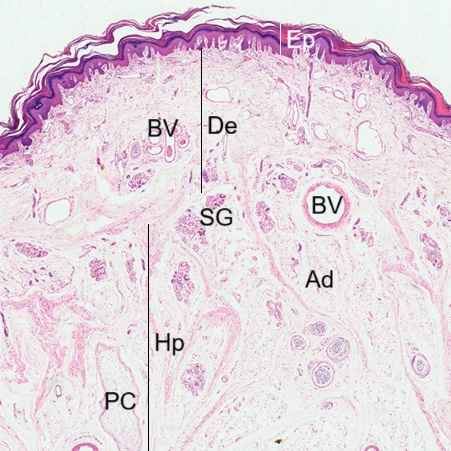
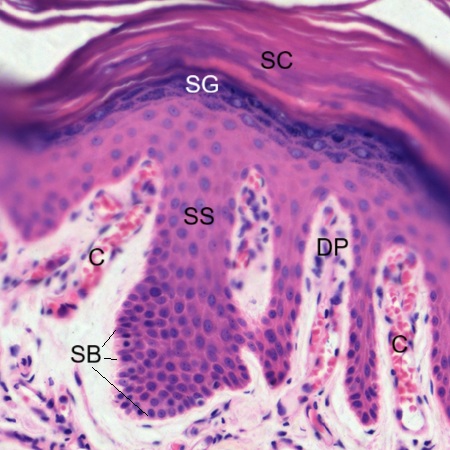
Thick skin is characterized by its five epidermal layers, including the extra stratum lucidum, which is unique to thick skin found on the palms and soles. In a section of sole skin stained by HE (Fig. 10-1), the typical three-layered structures are seen, including epidermis (Ep), dermis (De), and hypodermis (Hp). Apparently, the epidermis is thicker than the dermis. Most sweat glands (SG) are found between dermis and hypodermis. The hypodermis has abundant adipose tissue (Ad) with muscle bundles (M). In the other section of sole skin stained by HE (Fig. 10-2), the epidermis (Ep) is thinner than the dermis (De). Sweat glands are not only seen between dermis and hypodermis (SG1) but also seen in the hypodermis (SG2). Blood vessels (BV) are found but only few muscle bundles (M) are at the cut edge. Adipose tissue is only seen to be with sweat glands. As stated above, micrographs taken from two sections (Figs. 10-3 and 10-4) reveal that the epidermis is composed of stratified squamous keratinized epithelium dividing into five layers as follows:
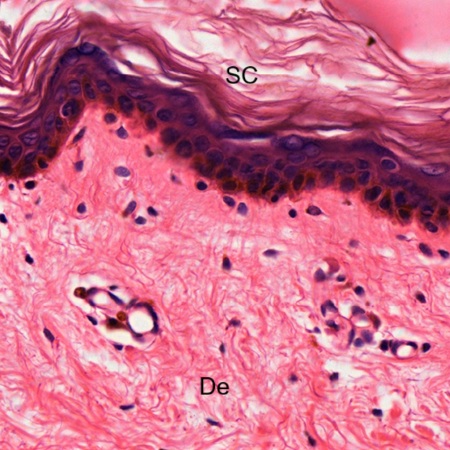
1) Stratum Corneum (SC) – a thick layer of dead cells devoid of nuclei and organelles.
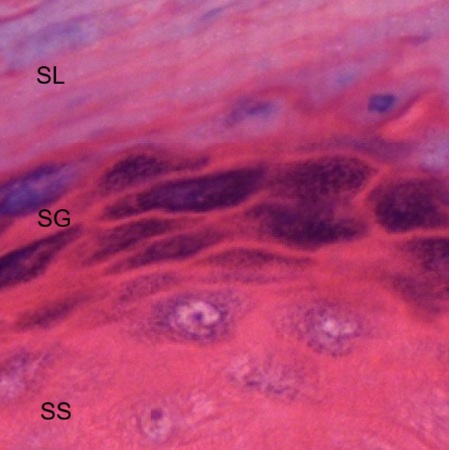
2) Stratum Lucidum (SL) – a highly refractive zone only seen in very thick skin (Fig. 10-5).
3) Stratum Granulosum (SG) – layers of keratinocytes with numerous basophilic, keratohyalin granules in their cytoplasm (Fig. 10-5).
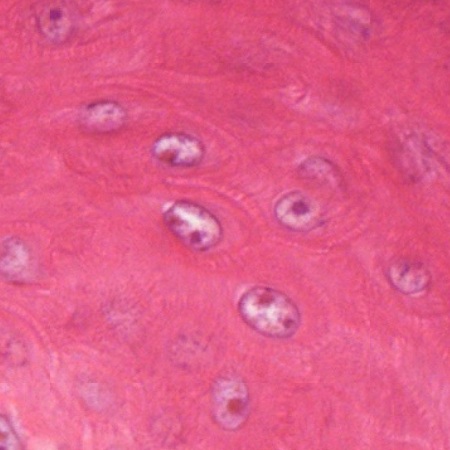
4) Stratum Spinosum (SS) – layers of keratinocytes attached to each other by desmosomes on spiny processes .( Figs. 10-5, 10-6, 10-7)
5) Stratum Basale (SB) – a single layer of germinal cells resting on the basement membrane (BM) which is attached to the dermis (Fig. 10-7).
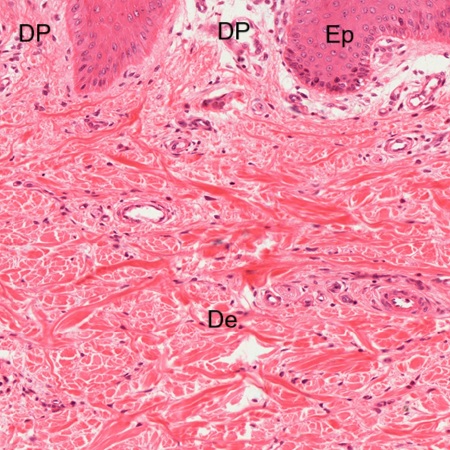
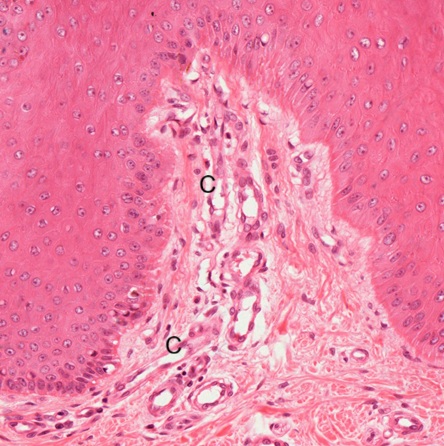
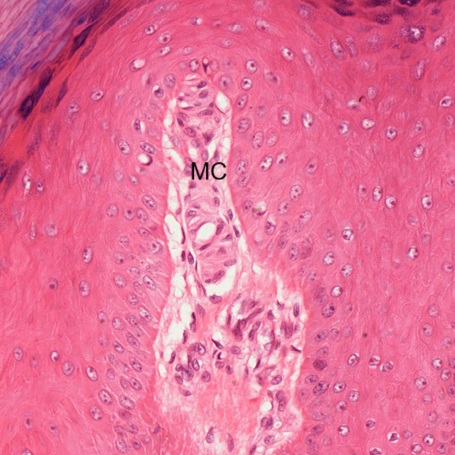
Dermis (De) is composed of dense irregular connective tissue. The border line between epidermis (Ep) and dermis is wavy to form dermal papillae (DP) into the epidermis (Fig. 10-8). Capillaries (C) are seen to enter into the dermal papillae (Fig. 10-9). In addition to the capillaries, Meissner’s corpuscles (MC) can be also found in the dermal papillae (Figs. 10-10 and 10-11). Detailed structure of the Meissner’s corpuscle has been illustrated in the chapter NERVOIUS TISSUE (Figs. 7-88, 7-89, 7-90).
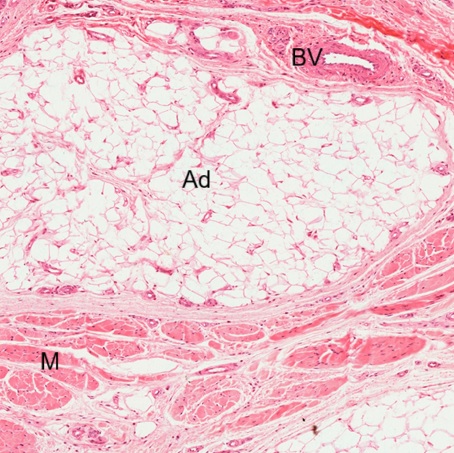
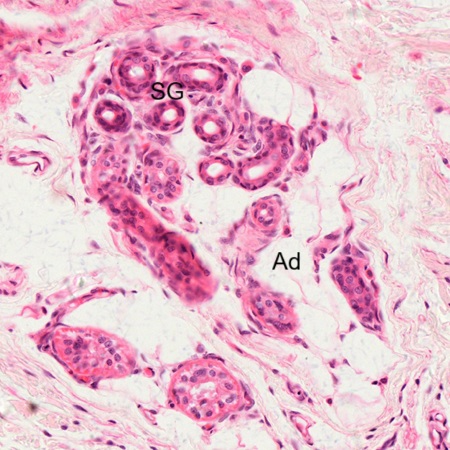
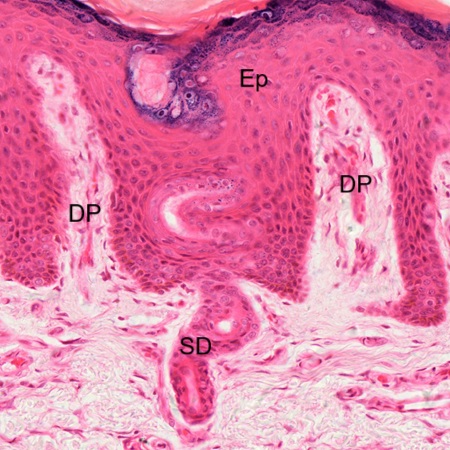
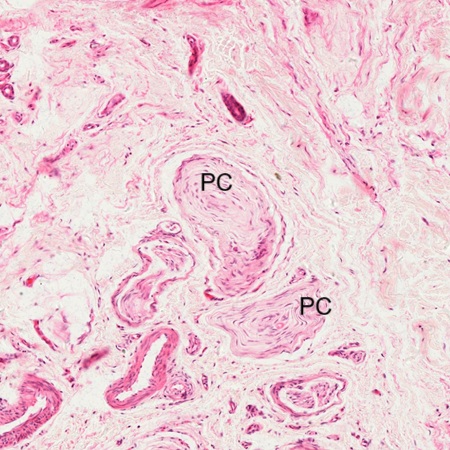
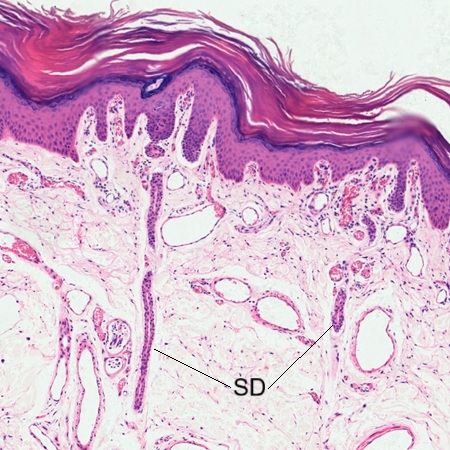
Hypodermis (Fig. 10-12) is composed of loose connective tissue with adipose tissue (AD). Blood vessels (BV) and muscle bundles (M) underneath the hypodermis are seen. As mentioned above, sweat glands (SG) can also be found to be with adipose tissue (Ad) in the hypodermis (Fig. 10-13). Sweat gland is a simple coiled tubular gland. Its secretary duct (SD) is found to spiral upwards (Fig. 10-14) and pierce through the epidermis (Ep) but not through the dermal papillae (DP). Two Pacinian corpuscles (PC) are also found in the hypodermis (Fig. 10-15). Detailed structure of the Pacinian corpuscle has been illustrated in the chapter NERVOIUS TISSUE (Figs. 7-91, 7-92, 7-93, 78-94).
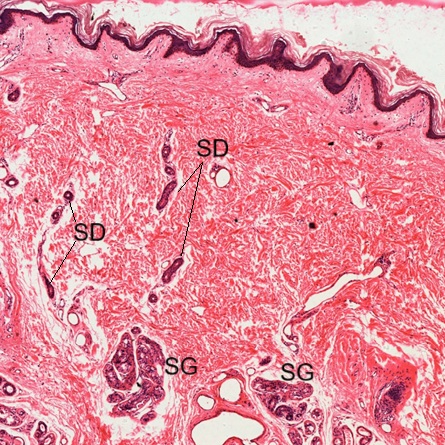
Thin skin is a type of skin found on most of the body, except for the palms and soles. A section of facial skin stained by HE (Fig. 10-16) reveals that the epidermis (Ep) is very thin relative to dermis (De) and hypodermis (Hp). There are sweat glands (SG) and blood vessels (BV) spreading within dermis and hypodermis. Pacinian corpuscles (PC) and adipose tissue (Ad) can be found in the hypodermis. The epidermis (Fig. 10-17) has four layers: the stratum basale (SB), stratum spinosum (SS), stratum granulosum (SG), and stratum corneum (SC). The refractive layer, stratum lucidum, is not seen. Many capillaries (C) are found in the dermal papillae (DP). Dermis is composed of dense irregular connective tissue (Fig. 10-18). Secretory ducts (SD) of sweat glands are seen to spiral upwards and pierce through the epidermis.
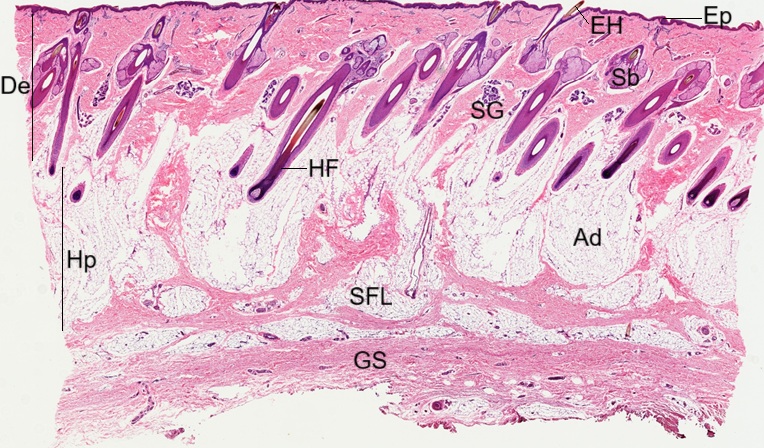
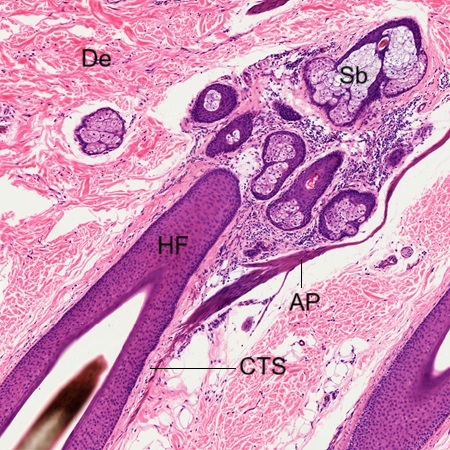
The above section is taken from facial area with no hair. In human most body skin, except palm and sole, usually contain hairs. In a section of hairy skin stained by HE (Fig. 10-19), it is found that the epidermis (Ep) is very thin relative to dermis (De) and hypodermis (Hp). The dermis is composed of dense irregular connective tissue while the hypodermis is composed of loose connective tissue. Many hair follicles (HF) and sweat glands (SG) can be seen in the dermis. The epidermis is too thin to distinguish between epidermal layers except the stratum corneum (SC), which is the outmost layer (Fig. 10-20). Compared to the above sections of other parts of skin, there are fewer dermal papillae found (Fig. 10-21). Capillaries (C) are seen entering into the dermal papillae. Sweat glands (SG) in the dermis are found sending out secretory ducts (SD) toward the epidermis .
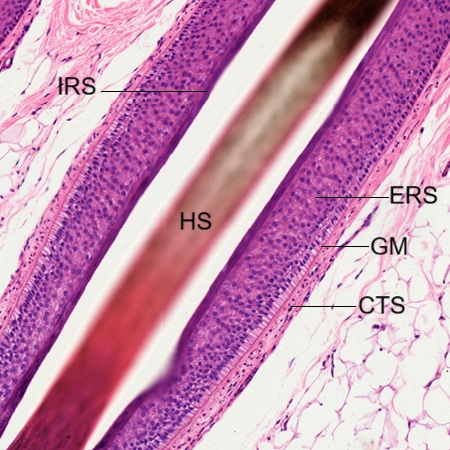
All hair follicles seen in this section are cut transversely at different points. The first micrograph (Fig. 10-23) shows the section through a hair root above hair bulb. The hair follicle is a tubular structure consisting of five layers of epithelial cells, including external root sheath (ERS), internal root sheath (IRS), cuticle (Cu), cortex (Cx), and medulla which is not seen in the section of a fine hair. The cortex is a broad, highly keratinized layer forming the bulk of the hair. Outside the cortex, a hard, thin cuticle is formed from keratinization. Between connective tissue sheath and external root sheath, there is a thick specialized basement membrane known as glassy membrane (GM). The entire hair follicle is surrounded by a connective tissue sheath (CTS) in the dermis (De). The internal root sheath can be further distinguished into three layers (Fig. 10-24): the outermost Henel’s layer (He), the middle Huxley’s layer (Hu), and the innermost cuticle layer (Cu-I) which is continuous with the cuticle (Cu) outside the cortex (Cx) of the hair root. The glassy membrane (GM) is clearly seen between the connective tissue sheath (CTS) and external root sheath (ERS).
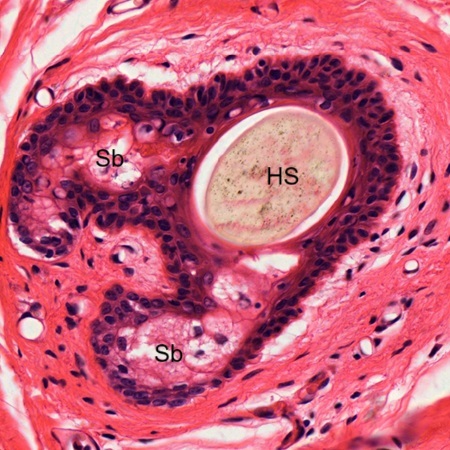
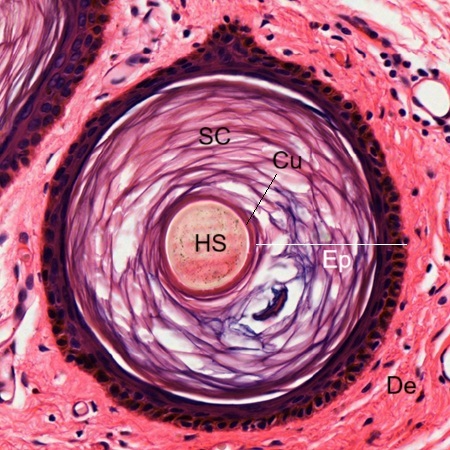
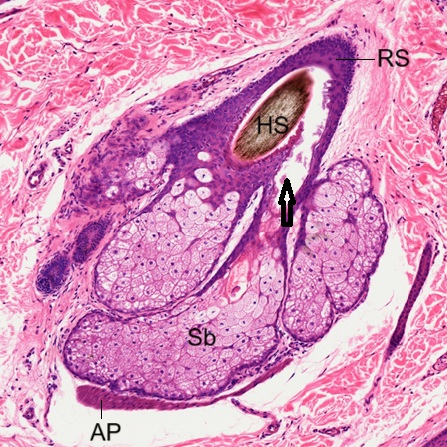
The micrograph shows the section of hair root cut at the point far from the hair bulb (Fig. 10-25). Visible layers surrounding the hair shaft (HS) include cuticle (Cu), internal root sheath (IRS), external root sheath (ERS), and connective tissue sheath (CTS). One section of hair root (Fig. 10-26) reveals sebaceous glands (Sb) appearing within epithelial layers of root sheath surrounding hair shaft (HS). The other section (Fig. 10-27) shows that the hair shaft (HS), which is covered by a layer of cuticle (Cu), has emerged from dermis (De) and is piercing through stratum corneum (SC) of the epidermis (Ep).
Scalp
The scalp is the area of the upper face covered by hair, consisting of five parallel layers: skin, superficial fatty layer, galea aponeurotica, loose areolar tissue, and periosteum. In a section of scalp (Fig. 10-28), three layers of skin structure, including epidermis (Ep), dermis (De), and hypodermis (Hp) are seen. The adipose tissue contained (Ad) in the hypodermis is continuous with superficial fatty layer (SFL) and galea aponeurotica (GA). Many hair follicles (HF) emerged hairs (EH), sebaceous glands (Sb), and sweat glands (SG) are seen. The scalp skin consists of the same five epidermal layers as seen in the thick skin (Fig. 10-29): stratum corneum (SC), stratum lucidum (SL), stratum granulosum (SG), stratum spinosum (SS), stratum basale (SB). Melanin granules produced by melanocytes are seen to be accumulated in the stratum basale. Dermis (De) is composed of dense irregular connective tissue.
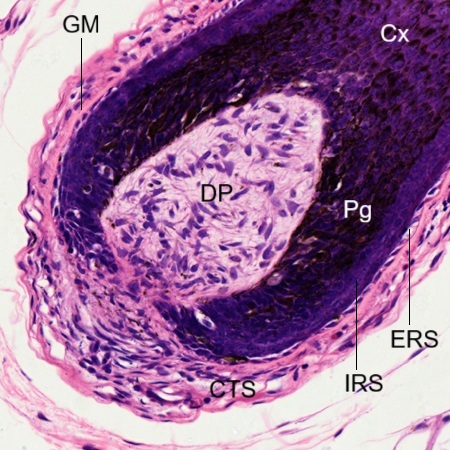
A longitudinal section of hair follicle reveals an enlarged hair bulb formed at its bottom end (Fig. 10-30). The hair bulb comprises the expanded portion of the inferior hair follicle and contains the dermal papilla (DP) and hair matrix. The dermal papilla consists of mesenchymal cells with blood vessels and nerve endings. The hair matrix consists of proliferating keratinocytes. These cells proliferate and gradually move upwards where they are keratinized to produce the hair shaft. Large amount of pigment (Pg), produced by melanocytes, are seen in the basal layer extending up into cortex (Cx). The melanocytes are derived from the stratum basale of epidermis. As seen in other part of the hair follicle, the entire hair bulb is surrounded by internal root sheath (IRS), external root sheath (ERS), glassy membrane (GM) and connective tissue sheath (CTS). Moving the observation field upward (Fig. 10-31), It reveals that the cortex (Cx) is the thickest layer of the hair shaft, made of densely packed, heavily keratinized cells that provide mechanical strength and color to the hair due to the presence of melanin pigment. Other layers of the hair follicle can be seen clearly, including cuticle (Cu), internal root sheath (IRS), external root sheath (ERS), glassy membrane (GM) and connective tissue sheath (CTS). Moving further upward, a nature space appears between hair shaft (HS) and root sheath. Layers of root sheath remain intact, including internal root sheath (IRS), external root sheath (ERS), glassy membrane (GM) and connective tissue sheath (CTS). At this point, the hair follicle is still in the hypodermis.
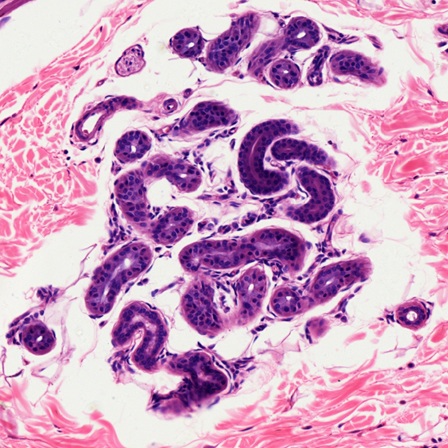
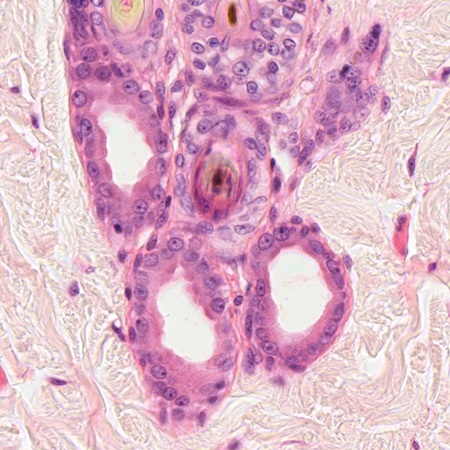
Once the hair follicle (HF) enters the dermis (De), sebaceous gland (Sb) and arrector pili (AP) appear to attach to it (Fig. 10-33). Arrector pili, also known as hair erector, is a group of smooth muscle fibers that are connected to the connective tissue sheath (CTS) of the hair follicle and extend towards the epidermis. These muscles are innervated by autonomic nerve fibers and are responsible for moving the hair, causing it to stand on end. Sebaceous glands (Sb) and arrector pili (AP) seem to have a locational relationship (Fig. 10-34). Sebaceous glands produce an oily substance called sebum. This sebum lubricates the skin and hair, protects against moisture and bacteria, and helps remove old skin cells. In this micrograph, their secretory ducts are seen to open into the nature space between hair shaft and root sheath. Sweat glands (SG) are also found around. In the other micrograph (Fig. 10-35), sebaceous gland (Sb) and arrector pili (AP) are shown. Secretory duct of the sebaceous gland is channeled to the nature space between hair shaft (HS) and root sheath (RS). The sebaceous glands are simple branched acinar glands. They release contents with the entire cells themselves, becoming part of the secretion in a way like other holocrine glands. The sweat glands (Fig. 10-36) of the scalp or other parts of the skin mentioned above are simple coiled tubular glands. They excrete products through exocytosis into the epithelial-walled ducts and then to lumen without causing any damage or loss in the secretory cell. Thus, they are merocrine glands, also known as eccrine glands.
Axillary Skin
A section of axillary skin stained by HE is shown here (Fig. 10-37). It is different from other parts of skin by a dense concentration of skin appendages, including numerous hair follicles (HF), sebaceous glands (Sb), and apocrine sweat glands (AS). A hair bulb (HB) is seen with apocrine sweat glands around. Some skeletal muscle bundles (SK) are found to extend from the underneath muscle layer (M) toward the epidermis. There are no arrector pili muscles in the axillary skin. Only apocrine sweat glands (AS) are seen but not eccrine sweat gland in this section. The axillary skin is a thin skin with thin epidermis and without stratum lucidum (Fig. 10-38). The most characteristic feature is the abundance of apocrine sweat glands (AS) associated with hair follicles (HF), which provide secretion channels (arrow) for both apocrine sweat glands (AS) and sebaceous glands (Sb) together (Fig. 10-39). Some skeletal muscle fibers (SK) are seen around. Histologically, apocrine sweat gland (Fig. 10-40) can be distinguished from eccrine sweat gland (Fig. 10-36) by its larger overall structure and lumen diameter.
Nipple
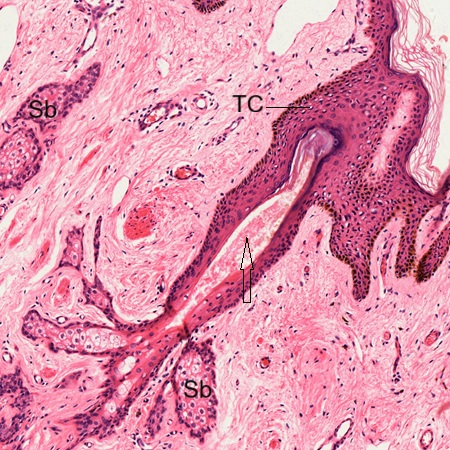
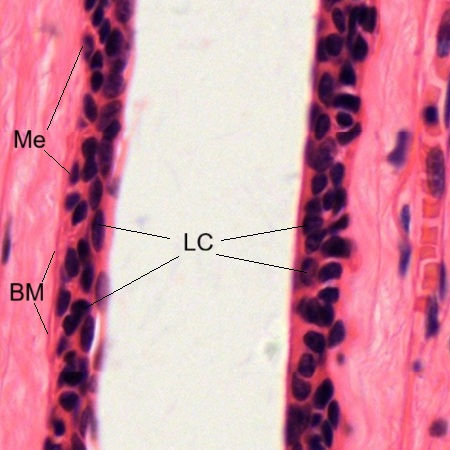
Nipple and surrounding areolar skin are specialized part of the skin. In section of nipple stained by HE (Fig. 10-41) reveals that it is covered with a stratified squamous keratinized epithelium (SSKE) and contain lactiferous ducts (LD) within dense fibrous stroma (DFS). Ostium (Os) of the lactiferous duct is seen on the skin surface. The epidermis contains a lot of clear keratinocytes or Toker cells (TC), which are believed to develop from sebaceous glands (Fig. 10-42). Sebaceous glands (Sb) are seen but hair follicles are absent. They may have their own excretory ducts (arrow) or share ostium with a lactiferous duct. The lactiferous duct (Fig. 10-43) is composed of a double-layered epithelium with luminal cells (LC) on the inside and myoepithelial cells (Me) on the outside, beneath a basement membrane (BM).
Nail
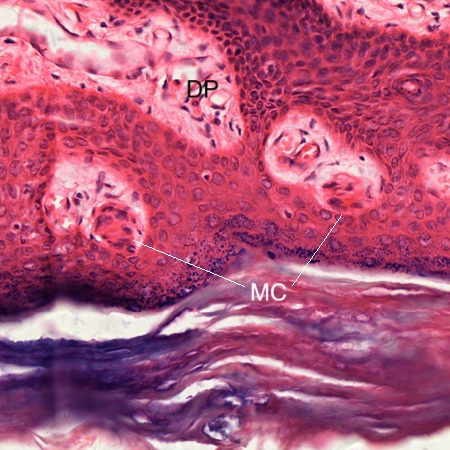
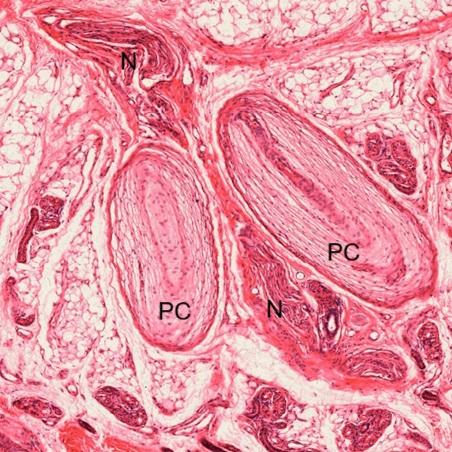
Nail is a highly specialized appendage formed on the dorsal skin surface of the tip of each finger and toe. A longitudinal section of infant finger stained by HE (Fig. 10-44) reveals that the nail is a highly keratinized structure located on the dorsal surface of the distal phalanx (DP), which has the hyaline cartilage (HC) covering proximal end articulated with the middle phalanx (MP). The horny nail plate (NP) extends deep into the dermis (De), forming the nail root (NR). The epidermis of the dorsal skin forms a continuous fold resulting in the eponychium (Ep), or cuticle, the nail bed (NB) underlying the nail plate, and the hyponychium (Hy). The epithelium (arrow) surrounding the nail root is responsible for the continuous elongation of the nail. In ventral skin (VS) of the finger, a lot of sweat glands (SG) are seen between dermis and hypodermis. In the hypodermis, many Pacinian corpuscles (PC), blood vessels (BV), and nerve bundles (N) are found to be surrounded by the adipose tissue (Ad). In the epidermis of ventral skin (Fig. 10-45), Meissner’s corpuscles (MC) are found to be located in the dermal papillae (DP). Two Pacinian corpuscles (PC) with nerve bundles (N) in between show typical onion-like structure (Fig. 10-46).
NOTE:
- Only those organelles visible under the light microscope are discussed here. It is suggested that to study all organelles visible under the electron microscope through your histology textbook and atlas.
- All photos used for discussion are taken from DSMH digital slides and other source as follows:
H080010 Thick Skin, sec. of sole skin, human, HE. (Figs. 10-1, 10-2, 10-3, 10-4, 10-5, 10-6, 10-7, 10-8, 10-9, 10-10, 10-11, 10-12, 10-13, 10-14, 10-15)
H080020 Thin Skin, sec. of facial skin, human, HE. (Figs. 10-16, 10-17, 10-18)
H080030 Scalp, sec., human, HE, showing hair follicles, sebaceous and sweat glands. (Figs. 10-28, 10-29, 10-30, 10-31, 10-32, 10-33, 10-34, 10-35, 10-36)
H080040 Nail, ls. of infant finger, human, HE, showing nail development. (Figs. 10-44, 10-45, 10-46)
H080050 Hairy Skin, sec. of body skin, human, HE. (Figs. 10-19, 10-20, 10-21, 10-22, 10-23, 10-24, 10-25, 10-26, 10-27)
H080060 Nipple, sec., human, HE. (Figs. 10-41, 10-42, 10-43)
H080070 Axillary Skin, sec. human, HE. (Figs. 10-37, 10=38, 10-39, 10-40) - Staining abbreviations and results:
HE = hematoxylin and eosin, is used to stain cell nuclei blue and cytoplasm pink or red. Hematoxylin may also stain ribosomes and rough endoplasmic reticulum blue.